THE SURFACES OF CELLS IN VARIOUS ORGANS
and tissues have receptor sites. Hormones and other
chemicals act at their respective receptor sites to bring
about a particular action in the cell. Adrenaline and
noradrenaline are called catecholamines and are released
from sympathetic nerve endings and as hormones from the
adrenal glands. They have their major actions on receptor
sites called beta-receptors. Stimulation of the sympathetic–
adrenal system during danger or severe stress, for example,
causes an outpouring of adrenaline and noradrenaline into
the blood circulation and at nerve endings.
Catecholamines (adrenaline and noradrenaline) are
stimulants and cause an increase in the force of contraction
of the heart increasing heart rate, blood pressure, and
blood sugar. An outpouring of catecholamines is necessary
to prepare the body for a fight-or-flight response.
Therefore, we need this surge of adrenaline if we have
to flee from a charging bull. Although adrenaline and
noradrenaline have positive effects, in excess they can cause
overcharging of the cardiovascular system, which can precipitate
ventricular fibrillation.
It is well documented that during a heart attack large
quantities of noradrenaline are released into the heart
muscle, which can precipitate abnormal heart rhythms,
particularly, ventricular fibrillation. Adrenaline causes an
increase in heart rate and an increase in blood pressure,
thus causing the heart to work harder. Because a coronary
artery is blocked during a heart attack, the increased work
with less available oxygen causes further damage to the
heart muscle and increases the size of the muscle damage,
causing a larger heart attack.
Beta-blocking drugs were originally discovered by
Sir James Black of Imperial Chemical Industries. Since
the introduction of the prototype, propranolol, for the
management of hypertension in 1964, more than 12 betablocking
drugs have become available. Beta-adrenergic
blocking drugs have become the cornerstone of cardiac
drug therapy.
I. BETA-RECEPTORS
By definition, beta-blockers block beta-receptors. Structurally
they resemble the catecholamines (adrenaline and
noradrenaline) and block the action of these catecholamines
at their receptor sites. The beta-receptors are
situated on the cell membrane and are believed to be a part
of the adenyl cyclase system. An agonist acting on its
receptor site activates adenyl cyclase to produce cyclic
adenosine-5-monophosphate, which is believed to be the
intracellular messenger of beta stimulation. There are two
types of beta-receptors, beta-1 and beta-2.
A. Beta-1 Receptors
The beta-1 receptors are present mainly in the heart,
renin-secreting tissues of the kidney, parts of the eye
responsible for the production of aqueous humor, and to a
limited degree in bronchial tissue of the lung. Beta-1-
adrenergic receptors regulate heart rate and myocardial
contractility, but in situations of stress with the provocation
of epinephrine release stimulation of cardiac beta-2
receptors contribute to additional increases in heart rate
and contractility.
B. Beta-2 Receptors
These are predominant in the bronchial tissues of the lung,
vascular smooth muscle, insulin-secreting tissues of pancreas,
gastrointestinal tract, and to a limited degree in
the heart and coronary arteries. None of these tissues
exclusively contains one subgroup of receptor. The population
density of receptors decreases with age. In addition,
the beta-receptor population is not static, and during
long-term therapy with beta-adrenergic blocking agents
the number of receptors is increased.
The heart contains beta-1 and beta-2-adrenergic
receptors in the proportion 70:30. In heart failure, cardiac
beta-1 receptors are reduced in number and population.
II. MECHANISM OF ACTION
Blockade of cardiac beta-1 receptors causes a decrease in
heart rate, myocardial contractility, and velocity of cardiac
contraction. Beta-blockers cause the heart muscle to work
less, thus requiring less oxygen; in time of oxygen lack,
such as during a heart attack or severe angina, this action
can be life-saving. Because of the reduction in the oxygen
requirement of the heart muscle, the beta-blocking drugs
are effective in preventing the chest pain of angina pectoris.
Because patients with angina have a high risk of developing
a heart attack over ensuing years, beta-blockers are
important for both pain and prevention.
An increase in adrenaline such as that produced during
stress or vigorous exercise causes an increase in (1) the
number and stickiness of blood platelets, (2) clotting factor
VIII (the hemophilic factor), and (3) the viscosity of
the blood. Beta-blockers block some harmful effects of
adrenaline.
Beta-blockers have antiarrhythmic effects; they depress
phase 4 diastolic depolarization and are effective in
abolishing arrhythmias caused by increased catecholamines.
This action is particularly important in patients
with ischemic heart disease. The electrical impulse traffic
through the AV node in reduced with beta-blockers and
the rate of conduction is slowed. This important action
slows the heart rate in patients with rapid heart rates
caused by atrial fibrillation. There is also a favorable effect
on ventricular arrhythmias, particularly those induced by
increased sympathetic activity observed in patients with
oxygen lack to the myocardium because of obstructive
coronary artery disease. Blockade of beta-1 receptors
reduces activity of the renin–angiotensin system in the
kidney by reducing renin released from the juxtaglomerular
cells; this action causes some lowering of blood
pressure.
Pierre-Yves et al. have shown that patients with stable
coronary artery disease exhibit much higher exercise
releases of atrial and ventricular natriuretic peptides
(ANP and BNP) when they are treated with beta-blockers
these authors postulated that increased secretion of potent
vasodilating and natriuretic agents constituted a mechanism
for protecting diseased hearts against stress.
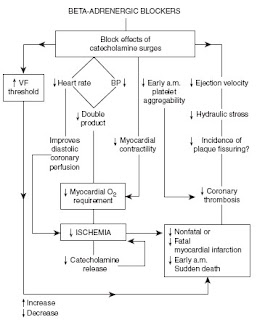
III. SALUTARY EFFECTS
Beta-blockers have been shown to prevent fatal and nonfatal
heart attacks and sudden cardiac death. (The salutary
effects of beta-adrenergic blockade are depicted in Fig. 1.
A decrease in heart rate increases the diastolic interval
during which the coronary arteries are filled with blood.
The coronary arteries are squeezed during systole and blood
flow is restricted. Thus beta-blockers increase oxygen
supply to the myocardium. This major beneficial effect has
not been given prominence by workers in the field.
Beta-blockers decrease the force and velocity of cardiac
contraction and decrease the heart rate pressure product
(RPP). This action decreases myocardial oxygen demand
and is important in the relief of angina.
It is interesting to note the good effect of beta-blockers
on the arterial system. The thousands of miles of arteries
are constantly under pressure from the pulsatile force and
velocity of blood as well as blood pressure. The decrease in
cardiac ejection velocity and a decrease in hemodynamic
stress on the arterial wall, especially at the branching of
arteries, may decrease the atherosclerotic process and
plaque rupture. Atherosclerosis is commonly seen where
arteries divide. Beta-blockers reduce blood pressure as
well as the force and velocity of blood flow at these
dividing points of mechanical stress and provide some
protection from vessel wall injury. This favorable effect is
of paramount importance in patients with high blood
pressure. Mechanical injury from the velocity and force of
blood is the prime cause of vessel wall injury, which leads
to atherosclerosis, dissection of the plaques of atheroma
and subsequent thrombosis, as well as rupture of an
aneurysm.
A decrease in the fatal arrhythmias, an increase in
ventricular fibrillation threshold, and amelioration of
ventricular and supraventricular arrhythmias have been
documented with beta-blockers. They decrease early
morning platelet aggregation and arrhythmias induced
by catecholamines. By doing this, they decrease the
early morning peak incidence of heart attack and sudden
death.
IV. INDICATIONS
A. Angina
Beta-blockers are first-line therapy for the management of
stable angina. They have been shown to be more effective
than oral nitrates and calcium antagonists. They reduce the
recurrence of chest pain in more than 66% of patients.
Many patients with angina manifest little pain, but they
may have several episodes of ischemia during the day or
night.These episodes can be adequately suppressed by
the use of beta-blocking drugs (see the chapter Angina).
In patients with unstable angina these drugs are used
immediately with aspirin when the patient arrives in the
emergency room.
B. Acute Myocardial Infarction
Beta-blockers are strongly recommended as therapy for
acute myocardial infarction and are administered within
minutes of arrival in the emergency room to virtually all
patients who present with acute chest pain believed to be
caused by a heart attack. As soon as an ECG confirms the
diagnosis, an aspirin, a beta-blocker, and a thrombolytic
agent are administered. In patients with acute myocardial
infarction beta-blockers have been shown to prevent
cardiac death and reduce infarct size. In these patients,
beta-blockers are often continued for several years.
C. Hypertension
Beta-blockers and diuretics remain first-line agents for the
management of virtually all patients with hypertension.
Beta-blockers are the drugs of choice in younger and older
white patients. Contrary to the opinion of some experts,
beta-blockers have been proven effective in older white
patients. Beta-blockers are particularly indicated in all
individuals with hypertension and concomitant coronary
artery disease, diabetes, or dyslipidemia. They are indicated
for hypertension in younger African-Americans;
they appear to be less effective in older patients of African
origin. (see the chapter Hypertension). Beta blockers are
also indicated in hypertensive patients with mild-tomoderate
heart failure.
D. Arrhythmias
Atrial fibrillation is the most commonsustained arrhythmia
observed in clinical practice and is a common disorder
observed worldwide. Beta-blockers remain the mainstay of
therapy to control the rapid heart rate in these patients.
These agents have replaced digoxin, except in patients with
severe heart failure. In a few patients paroxysmal attacks
may be prevented (see the chapter Atrial Fibrillation).
Ventricular premature beats, particularly those caused
by coronary artery disease and mitral valve prolapse, are
another type of arrhythmia. Nonsustained ventricular
tachycardia may respond to beta-blockers in patients
with coronary artery disease and repetitive ventricular
fibrillation caused by electrocution.
E. Heart Failure
The harmful effects of overactivation of the sympathetic
nervous system in heart failure are ameliorated significantly
by beta-blockers. The judicious use of titrated doses of
beta-adrenergic blockers has been shown to improve
quality of life, recurrence of heart failure, and mortality
in patients with various grades of heart failure. The
COPERNICUS study involved 2289 patients with severe
heart failure and ejection fractions of less than 20%.
The treatment drug carvedilol caused significant reductions
in mortality and hospitalization for heart failure. The
COMET study randomized 1511 patients with chronic
heart failure (ejection fraction less than 35%) to treatment
with carvedilol and 1518 to metoprolol. Follow up at
58 months showed all-cause mortality to be 34% for
carvedilol and 40% for metoprolol, p¼0.0017.
F. Elective Percutaneous Coronary
Intervention
Elective percutaneous coronary intervention (PCI) involving
balloon angioplasty and intracoronary stent implantation
is now done in many centers worldwide for the
management of coronary artery disease. All patients
undergoing PCI are administered beta-blocking drugs
that are continued indefinitely. A clinical trial has shown
that beta-blocker therapy is associated with a marked longterm
survival benefit among patients undergoing successful
PCI. Beta-blocker therapy has been shown to be associated
with a reduction from 6 to 3.9% at one year (P¼0.0014).
G. Dissecting Aneurysm
A dissecting aneurysm of the aorta is a life-threatening
condition resulting in death in greater than 75% of
patients. A beta-adrenergic blocking agent is the drug of
choice to reduce aortic pressure which decreases the rate
of dissection. A beta-blocker is often combined with
nitroprusside to lower blood pressure, but even when the
systolic blood pressures is as low as 110 mmHg, a betablocker
is still indicated to reduce cardiac ejection velocity
and thus the aortic pressure.
H. Mitral Regurgitation and Mitral Stenosis
Recent clinical trials with carvedilol in patients with mitral
regurgitation have documented improvement in geometry
of the left ventricle. In mitral regurgitation (a leaky valve),
blood flows backward through the widely opened valve
that should be shut and flows from the left ventricle into
the left atrium. The left ventricle becomes enlarged and
finally weakens causing heart failure. In an animal study of
mitral regurgitation, the ACE inhibitor, lisinopril, reduced
pre- and afterload, but its effect on the left ventricular
contractility was insignificant. Atenolol, when added to
lisinopril, achieved a maximum hemodynamic benefit
and also restored left ventricular contractility. Moderateto-
severe mitral regurgitation is an extremely difficult
condition to manage; the timing for surgery in patients
with severe disease is often a dilemma. Any cardioactive
agent that causes amelioration of the disease process is a
welcome addition to the drug armamentarium.
Beta-blockers are the cornerstone of treatment for
pregnant patients with moderate-to-severe mitral stenosis.
These agents slow the heart rate which allows filling of the
left ventricle and prevents life-threatening pulmonary
edema. In mitral stenosis the mitral valve opening is
stenosed or tight, and blood flow from the left atrium
is restricted. This flow is further decreased when the
heart rate is fast. Patients with mitral valve prolapse
and bothersome palpitations respond favorably to betablockers.
I. Hypertrophic Cardiomyopathy
Although medical treatment with beta-blockers does not
cause a decrease in mortality, symptoms are often significantly
relieved with a beta-blocking agent. See chapter
entitled ‘‘Cardiomyopathy.’’
J. Perioperative Mortality
Beta-blockers have been shown to decrease morbidity and
mortality in patients undergoing coronary artery bypass
surgery and in cardiac patients undergoing other types of
surgery. Beta-adrenergic blockade allows safer induction of
anesthesia and prevents the hypertensive response to
endotracheal intubation. These agents reduce the occurrence
of arrhythmias in the intra- and postoperative
periods. Both atenolol and bisoprolol have been shown
in randomized clinical trials to reduce morbidity and
mortality when given perioperatively and for one week
postoperatively.
K. Marfan Syndrome
This disease often causes dilatation of the ascending aorta,
which results in aortic dissection. Prophylactic betaadrenergic
blockade slows the rate of aortic dilation and
retards the development of aortic complications.
L. Diabetic Patients
Death in the majority of patients with type 2 diabetes is
caused by cardiovascular disease. Both fatal and nonfatal
and sudden heart attacks are common in diabetics.
Unfortunately, the usual optimal treatment of diabetes
with insulin or oral agents does not significantly prevent
cardiovascular complications. Beta-adrenergic blockers are
usually considered by experts to be relatively contraindicated
in diabetics, particularly those with dyslipidemias.
This expert advice is illogical. These are the only
cardioactive agents along with aspirin that could protect
the heart from serious events and dyslipidemia can be
controlled with statins. (See the chapter Diabetes). Also,
beta-blockers appear to have a renoprotective effect. In the
SOLVD heart failure study, surprisingly in contrast to the
ACE inhibitor enalapril, beta-blockers were renoprotective
in both the ACE inhibitor and the placebo groups. See the
later discussion of the UKPDS beneficial results in
diabetics treated with a beta-blocker in Section V.D.
M. Other Indications
Prolonged QT interval syndromes may cause syncope or
sudden death and beta-blockers provide some benefit in
these patients. An electrical storm in the heart may
precipitate multiple episodes of ventricular tachycardia or
ventricular fibrillation and repetitive ventricular fibrillation
resistant to therapy. The beneficial effect of the betablocker
propranolol on recurrent ventricular fibrillation
caused by electrocution was documented in 1970s, but
little attention was given to this report. Recent studies
have documented the role of beta-blockers in electrical
storms and today propranolol is used for the management
of repetitive ventricular fibrillation resistant to
defibrillation.
ADVERSE EFFECTS AND CAUTIONS
Beta-blockers are safe cardioactive agents if the warnings
and contraindications are followed. They are not advisable
in patients with severe class IV heart failure. They are indicated,
however, in class I–III heart failure. Class IV patients
who have been stabilized and are no longer decompensated
can be started on very small doses of carvedilol (3.5 mg).
Beta-blockers are contraindicated in patients with
bronchial asthma and in patients with severe chronic
obstructive pulmonary disease including emphysema.
Patients with mild chronic bronchitis may be given a
cardioselective beta-1 agent and may require supplemental
salbutamol. Other contraindications include:
1. Complete heart block and varying grades of heart block
2. Severe bradycardia less than 48 beats per minute
3. Allergic rhinitis
4. Insulin-dependent diabetics who are prone to hypoglycemia
5. Raynaud’s phenomenon
Adverse side effects of beta-blockers include tiredness
and fatigue in about 10% of patients, erectile dysfunction
in about 10%, precipitation of heart failure in patients
with poor left ventricular function, slowing of the heart
rate causing bradycardia less than 50 beats per minute,
depression in less than 5%, very cold extremities in less
than 10%, and vivid dreams. Switching to a hydrophilic
drug excreted by the kidney may decrease vivid dreams.
VII. CLASSIFICATION
A classification of beta-blockers is given in Fig. 3. Cardioselectivity
indicates that the drug chiefly blocks beta-1
receptors in the heart and partially spares beta-2 receptors
in the lungs and blood vessels. Large doses of all betablocking
agents block beta-2 receptors, thus, cardioselective
drugs are not cardiospecific. Bisoprolol is more
cardioselective than metoprolol or atenolol. The classification
into cardioselective and nonselective is important, but
oversimplified.
INDIVIDUAL BETA-BLOCKERS
A. Acebutolol
This relatively cardioselective, partially hydrophilic and
lipophilic agent possesses mild beta-agonist activity.
A dosage of 200–300 mg twice daily is given for hypertension.
Because of the presence of beta-agonist activity,
this drug is not indicated for the management of angina or
myocardial infarction.
B. Atenolol
This beta-1 cardioselective agent is water-soluble, hydrophilic,
and eliminated by the kidneys. It has a low side
effect profile and is therefore widely used. As outlined
above, the drug has not been shown to decrease mortality
in randomized trials. A dosage of 25–50 mg once daily is
given, but a dose of 75 mg is required in some patients
with angina or hypertension.
C. Bisoprolol
This agent is highly beta-1 selective and is more cardioselective
than metoprolol and atenolol. It is 50%
lipophilic and metabolized in the liver. The water-soluble,
hydrophilic component is excreted by the kidneys. The
concentration of unchanged bisoprolol in rat brain is lower
than that of metoprolol or propranolol, but higher than
that of atenolol after dosing. This agent has a low side
effect profile. A dosage of 5–10 mg once daily, and a
maximum of 15 mg daily is recommended.
D. Carvedilol
This noncardioselective agent is a beta-1, beta-2 receptor
blocker with very mild alpha-1 vasodilating activity.
A recent randomized trial has shown the drug to be
effective in reducing mortality in patients with acute
myocardial infarction with an ejection fraction of less
than 40%. In a large, randomized trial the drug significantly
decreased mortality and morbidity in patients
with moderate and severe heart failure. Patients are given a
dosage of 3.125 mg daily for heart failure, titrated slowly
over weeks to 12.5–25 mg twice daily. For hypertension
the dosage is 12.5 mg then 25 mg, if necessary, with a
maximum of 50 mg daily.
E. Metoprolol
This beta-1 cardioselective agent has been used extensively.
It is commonly used in the management of angina,
hypertension, and heart failure; clinical trials have shown
the drug to be effective in reducing morbidity and
mortality in patients with a moderate degree of heart
failure. Metoprolol is commonly prescribed to reduce the
rapid heart rate in patients with atrial fibrillation, but
other beta-blockers have similar effects.
F. Nebivolol
Nebivolol is a new, highly selective beta-1 receptor
antagonist with antioxidant properties that has been
shown to cause vasodilatation in humans. This agent
reverses endothelial dysfunction in hypertensive patients.
It appears that the drug causes vasodilatation through an
endothelial beta-2-adrenergic receptor mediated nitric
oxide production. Nitric oxide formed in arteries causes
salutary vasodilatation. The vascular release of superoxide
is increased in atherosclerotic arteries and oxygen can
inactivate nitric oxide; oxidative inactivation of nitric
oxide is a cause of endothelial dysfunction. Cominacini
et al. has shown that nebivolol increases nitric oxide by also
decreasing its oxidative inactivation.
G. Others
Other agents include the well known propranolol, but its
efficacy is questionable and should become obsolete for the
management of hypertension, angina, and following
myocardial infarction, because the other agents described
above cause less adverse effects. Sotalol is indicated mainly
for the management of some patients with paroxysmal
atrial fibrillation to maintain sinus rhythm.
For more information visit Jigfo.com, the no.1 source of information.




No comments:
Post a Comment